Experimental vaccines and therapeutics to combat the deadly Marburg virus will begin arriving this weekend in Rwanda, where they will be used in clinical trials expected to begin soon, a U.S. government official confirmed on Friday.
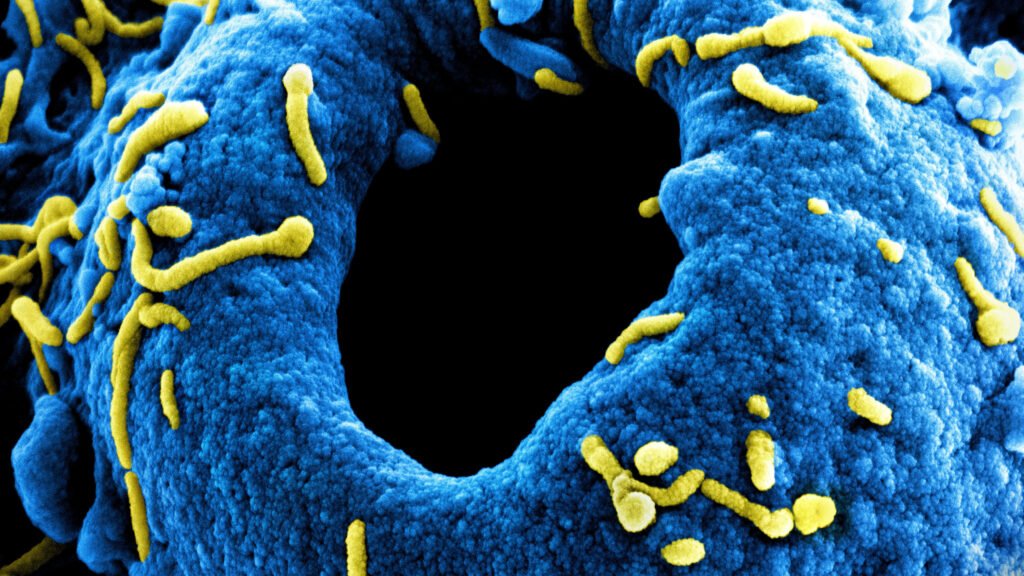
There are currently no licensed vaccines or drugs to prevent or treat Marburg, a cousin of the Ebola family of viruses that transmits and causes illness in the same way as Ebola. Although Marburg outbreaks are typically smaller, the fatality rates of the two infections are similarly high.
Rwanda has never before dealt with a Marburg outbreak, and the case count has already reached 41, making it one of the largest on record. Twelve of those people have died. More than 80% of the detected cases are in health care workers, many of whom were infected at a major health facility in the capital, Kigali.
The country has agreed to conduct clinical trials and has indicated it is ready to move quickly.
“We are aiming to start within days,” Health Minister Sabin Nsanzimana said Thursday during a press conference organized by the Africa Centres for Disease Control and Prevention. “We are talking about saving lives of health care providers.”
Nsanzimana sidestepped questions about the design of the trials — in other words, whether multiple vaccines or therapeutics could be used and compared with one another or whether they would be compared with a placebo.
It appears there will be at least two therapeutic options available in the country — Gilead Sciences’ antiviral drug remdesivir and Mapp Biopharmaceutical’s experimental monoclonal antibody MBP-091.
Remdesivir is approved in the United States as a treatment for Covid-19 and has been tested before as a therapeutic for Ebola. Nsanzimana said Gilead is providing 5,000 doses of the drug, which is sold commercially as Veklury.
A spokesperson for the Administration for Strategic Preparedness and Response — a division of the Department of Health and Human Services — said the U.S. government is supplying doses of vaccine and the monoclonal antibody. Both are being developed with the financial support of the Biomedical Advanced Research and Development Authority, or BARDA.
The single-dose vaccine was originally designed at the National Institutes of Health’s Vaccine Research Center and is now being developed by the nonprofit Sabin Vaccine Institute. The institute said it will be sending 700 doses of the vaccine.
Although there are several experimental vaccines to protect against Marburg in development, the Sabin vaccine is believed to be the furthest along in the pipeline. The institute is currently conducting a Phase 2 trial in Uganda and Kenya.
Nancy Sullivan, director of Boston University’s National Emerging Infectious Diseases Laboratories, led the research to design the vaccine in a previous job, at the VRC. She has also played a role in the extensive work the World Health Organization and partners have conducted in recent years to be ready to move quickly to test vaccines and drugs for rare diseases like Marburg, when the need arises.
“I’m gratified that the work that WHO has done has put the field in the position to be able to respond to an outbreak,” Sullivan told STAT.
Amy Finan, CEO of the Sabin Vaccine Institute, agreed that the preparatory work appears to be paying off here.
“I think there are a number of pieces that came together in order to move at lightning speed,” Finan said, noting that because the vaccine is already in a Phase 2 trial elsewhere, the documentation needed to start a new trial is in hand.
Another advantage: The institute had doses of the vaccine that could be used, which is not always the case for an experimental vaccine. IAVI — the International AIDS Vaccine Initiative — is also developing a Marburg vaccine, but it is in the process of making doses and has none to send.
Oxford University’s Oxford Vaccine Center, which designed what became AstraZeneca’s Covid-19 vaccine, is also developing a Marburg vaccine. STAT reached out to ask the status of its efforts and whether it has doses it could supply to Rwanda, but had not yet received a reply.
Finan also credited Rwanda for moving swiftly to try to extinguish this outbreak, which was first confirmed at the end of last week.
“Another huge important factor that I can’t overstate is the partnership with the Rwandan government,” Finan said. “Rwanda has the health infrastructure to support being able to move quite quickly. And I think that has really helped us.”
Share this content: